What Are Details of the Vascular TOS
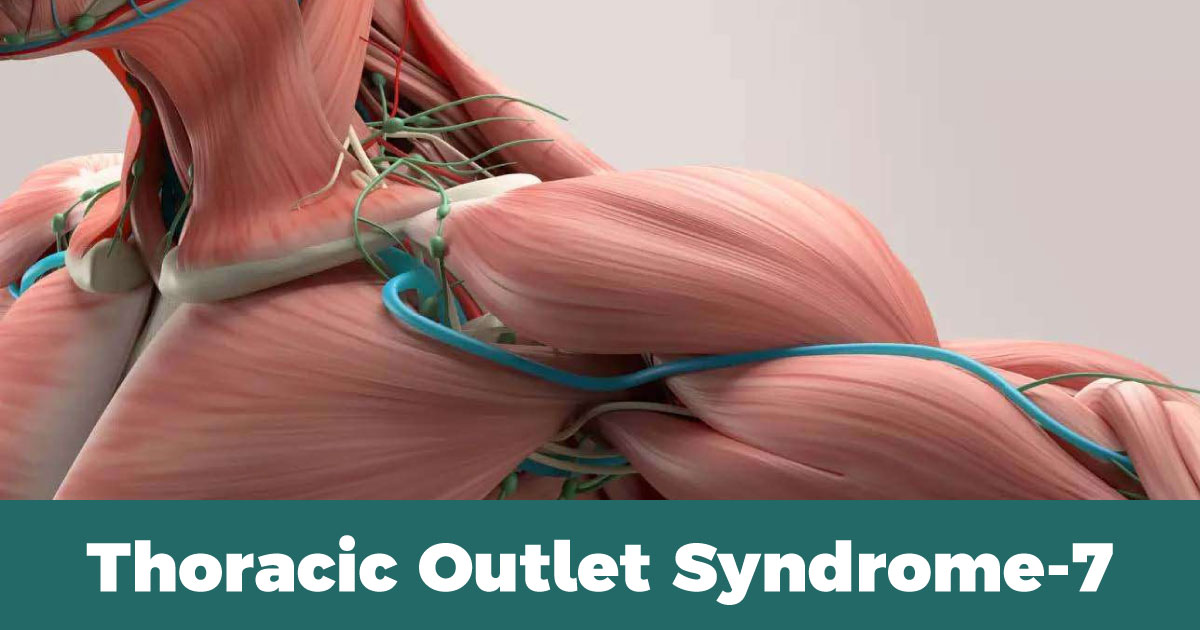
Vascular TOS is a less common type of TOS that is caused by compression of the blood vessels that run through the thoracic outlet. This can lead to restricted blood flow to the arm and hand, causing a range of symptoms.
The most common cause of vascular TOS is an abnormality in the first rib or an extra cervical rib, which can put pressure on the blood vessels as they pass through the thoracic outlet. Other causes may include trauma, postural abnormalities, or tumors.
Symptoms of vascular TOS may include:
- Pain, tingling, or numbness in the arm or hand
- Weakness or fatigue in the arm or hand
- Coldness or discoloration of the arm or hand
- Swelling of the arm or hand
- A weak or absent pulse in the affected arm
Diagnosis of vascular TOS typically involves imaging studies such as an ultrasound, magnetic resonance imaging (MRI), or angiogram to evaluate the blood vessels and identify any areas of compression or blockage. Treatment may involve medications to improve blood flow, physical therapy to improve posture and relieve pressure on the affected blood vessels, or surgery to remove the source of compression. In some cases, a combination of these approaches may be recommended.
What is Non-specific TOS
Non-specific TOS is a term used to describe a form of thoracic outlet syndrome (TOS) where the cause of compression cannot be clearly identified. This can make it challenging to diagnose and treat effectively.
Symptoms of non-specific TOS are similar to those of other forms of TOS and may include pain, numbness, tingling, or weakness in the neck, shoulder, arm, or hand. However, because the cause of the compression is unclear, the symptoms may be more difficult to attribute to TOS and may be mistaken for other conditions such as carpal tunnel syndrome, cervical radiculopathy, or fibromyalgia.
Diagnosis of non-specific TOS may involve ruling out other potential causes of symptoms through a variety of imaging tests and physical exams. Treatment for non-specific TOS may involve a combination of physical therapy, medications, and lifestyle changes such as improving posture and avoiding activities that exacerbate symptoms. In some cases, surgery may be recommended to relieve pressure on the affected nerves and blood vessels. However, the success rate of surgical intervention for non-specific TOS is less clear than for other forms of TOS, and therefore, it is typically reserved for cases that do not respond to other forms of treatment.
Idiopatic TOS and Possible Other Factors about Similar Symptoms
Idiopathic TOS is a form of thoracic outlet syndrome (TOS) where the cause of compression cannot be identified. The term “idiopathic” means that the condition arises spontaneously or for unknown reasons.
Symptoms of idiopathic TOS are similar to other forms of TOS and may include pain, numbness, tingling, or weakness in the neck, shoulder, arm, or hand. However, because the cause of compression is unclear, it can be challenging to diagnose and treat effectively.
In addition to idiopathic TOS, there are other conditions that can cause similar symptoms, such as carpal tunnel syndrome, cervical radiculopathy, cubital tunnel syndrome, and ulnar nerve entrapment. These conditions can also cause pain, numbness, tingling, or weakness in the arm or hand, and may be misdiagnosed as TOS.
To diagnose idiopathic TOS, a thorough medical history and physical examination are necessary, including specific tests to assess nerve and blood vessel function. Imaging tests such as X-rays, MRI, and ultrasound may also be used to confirm the diagnosis.
Treatment for idiopathic TOS may involve a combination of physical therapy, medications, and lifestyle changes such as improving posture and avoiding activities that exacerbate symptoms. Surgery may also be recommended in some cases, but the success rate is less clear than for other forms of TOS.
In summary, idiopathic TOS is a form of TOS where the cause of compression cannot be identified. The symptoms of idiopathic TOS may be similar to other conditions that cause nerve and blood vessel compression, and a thorough evaluation is necessary to arrive at an accurate diagnosis.
TOS Similar Pathologies in the Brachial Plexus Neuralgia
Brachial plexus neuralgia is a type of neuropathic pain that arises from the irritation or compression of the brachial plexus, a network of nerves that supplies the upper limb. This condition may have some overlapping symptoms with thoracic outlet syndrome (TOS) and is sometimes mistaken for TOS. However, there are some distinguishing features that help differentiate the two conditions.
One key difference is that brachial plexus neuralgia typically involves pain and numbness that radiates down the arm, while TOS pain tends to be more localized to the shoulder, neck, and upper back. Additionally, brachial plexus neuralgia may be caused by trauma, infection, or nerve damage, whereas TOS is typically associated with anatomical abnormalities or compression of nerves or blood vessels in the thoracic outlet.
Treatment for brachial plexus neuralgia may involve medications to manage pain and inflammation, physical therapy to improve range of motion and strengthen the affected muscles, and in some cases, surgical intervention to address nerve compression or damage.
Causes of the Brachial Plexus Neuralgia
The causes of brachial plexus neuralgia can vary, but some possible factors include:
- Trauma: Trauma to the brachial plexus, such as from a motor vehicle accident or sports injury, can cause nerve damage or irritation that leads to neuralgia.
- Repetitive motions: Repetitive movements of the arms and shoulders, such as those involved in certain sports or work activities, can cause chronic irritation or compression of the brachial plexus.
- Infection: Certain infections, such as shingles or Lyme disease, can affect the nerves and cause neuralgia.
- Tumors: Tumors that develop near the brachial plexus can cause nerve compression and lead to neuralgia.
- Autoimmune disorders: Some autoimmune disorders, such as rheumatoid arthritis or lupus, can cause inflammation and damage to the nerves.
- Idiopathic: In some cases, no clear cause of brachial plexus neuralgia can be identified, and it is referred to as idiopathic neuralgia.
Infections Causing Brachial Plexus Neuralgia (See Details)
Some infections that can cause brachial plexus neuralgia include:
- Herpes zoster (shingles): This is a viral infection that affects the nerves and skin, and can cause severe pain and inflammation along the affected nerve pathway.
- Lyme disease: This is a bacterial infection that is spread by tick bites and can cause nerve inflammation and damage.
- HIV/AIDS: This virus can affect the nerves and cause inflammation and damage.
- Syphilis: This is a bacterial infection that can cause nerve damage and lead to neuralgia.
- Tuberculosis: This is a bacterial infection that can affect the nerves and cause inflammation and damage.
It’s important to note that these infections are relatively rare causes of brachial plexus neuralgia, and most cases are due to other factors such as trauma or repetitive motions. If you are experiencing symptoms of brachial plexus neuralgia, it’s important to see a healthcare professional for a proper diagnosis and treatment.
Tumors and Cancers Can Cause Braichial Plexux Neuralgia (See Details)
Tumors and cancers can also cause brachial plexus neuralgia, although they are less common than other causes. Tumors can directly compress or invade the brachial plexus, leading to nerve damage and pain. Some common types of tumors that can cause brachial plexus neuralgia include:
- Pancoast tumors: These are tumors that develop in the upper part of the lungs and can invade the brachial plexus, causing severe pain in the shoulder and arm.
- Neurofibromas: These are benign tumors that develop on the nerve sheaths of the brachial plexus and can cause nerve compression and pain.
- Metastatic tumors: These are cancers that have spread from other parts of the body to the brachial plexus and can cause nerve damage and pain.
Treatment for brachial plexus neuralgia caused by tumors may involve surgery to remove the tumor, radiation therapy, or chemotherapy. Pain management may also be necessary to control symptoms.
Autoimmune disorders can cause Brachial Plexus Neuralgia (See Details)
Autoimmune disorders can cause brachial plexus neuralgia by causing inflammation in the brachial plexus, leading to nerve compression and irritation. Examples of autoimmune disorders that can cause brachial plexus neuralgia include lupus, rheumatoid arthritis, and Sjogren’s syndrome. In these conditions, the immune system mistakenly attacks healthy tissues and organs, including the nerves in the brachial plexus. The resulting inflammation can cause pain, weakness, and numbness in the affected arm and hand, similar to the symptoms of brachial plexus neuralgia. Treatment for autoimmune-related brachial plexus neuralgia typically involves addressing the underlying autoimmune disorder with medication and other therapies to manage pain and inflammation.
Idiopathic Pathologies that cause Braichial Plexus Neuralgia
In some cases, the cause of brachial plexus neuralgia is unknown, which is referred to as idiopathic brachial plexus neuralgia. This can be frustrating for patients, as it is difficult to determine the best course of treatment without a clear understanding of the underlying cause. However, there are still treatment options available to manage symptoms and improve quality of life for those with idiopathic brachial plexus neuralgia.
Treatment Options About TOS
The treatment options for thoracic outlet syndrome (TOS) depend on the underlying cause and the severity of the symptoms. Here are some possible treatment options:
- Physical therapy: Stretching and strengthening exercises can help improve posture, reduce compression, and alleviate symptoms.
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants may help relieve pain and inflammation.
- Surgery: In some cases, surgery may be necessary to relieve compression and alleviate symptoms. The type of surgery will depend on the specific location and cause of the compression, and may include removal of a cervical rib, decompression of nerves, or removal of tumors.
- Lifestyle changes: Avoiding activities that aggravate symptoms, maintaining good posture, and adjusting workstations and sleeping positions may help alleviate symptoms.
- Alternative therapies: Acupuncture, chiropractic care, and massage therapy may help relieve pain and tension in some cases.
It is important to consult with a healthcare provider for proper diagnosis and treatment recommendations, as TOS can be a complex condition with multiple underlying causes.
Keywords: Thoracic Outlet Syndrome, TOS, brachial plexus, nerves, anatomy, scalene muscle, cervical rib, first rib, costoclavicular syndrome, Pancoast tumor, neurofibroma, hematomas, Vascular TOS, Neurogenic TOS, Non-specific TOS, Brachial Plexus Neuralgia, treatment options, physical therapy, surgery, occupational therapy, chiropractic care, acupuncture, medications.
Last Revision: 10.03.2023